by Monica Williams-Murphy, MD
Reprinted from Dr. Williams-Murphy’s blog at www.oktodie.com/blog
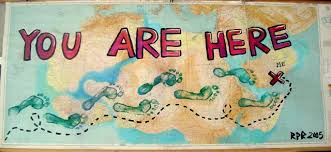
When you set out on an unfamiliar journey, you will need a map to get to your desired destination. You may pass landmarks, but not know exactly where you are unless you are able to identify these landmarks on your map. The same is true for the journey of life, and specifically, the path at the end of life.
You may know where you want the path to end (almost instinctively in the home), but unless someone can identify the landmarks for you (i.e. the physical signs of dying), then you may be unable to make the necessary turns and maneuvers to end up where you want to be.
What follows are three patient stories which illustrate the value of a “map” and knowing where you are on your journey toward the end of life:
Each of these stories begins the same way: The patient arrives to the ER. I talk to the patient and the family, and perform an examination, discovering that the patient appears to be in the last months or weeks of life due to some identifiable landmarks (which will appear in italics). I then sit everyone down for a “Where we are on the map” conversation in which I identify the patterns that suggest that the patient has entered their end-of-life pathway. In each case, I attempt to draw the “time line of life” in visual map-form for them, and then point out how close the patient is to the end, to the destination.
This knowledge frequently changes everything…
Patient 1- Mrs. Wiggins was 89 years old and up until 4 months ago had lived independently in her own home, but then she started falling. Then she stopped walking. Then she stopped eating. Because no one had given Mrs. Wiggins and her family “the map,” the family had chosen to place her in a Rehabilitation facility and now she had a special IV line in through which she was receiving artificial nutrition, and plans were to have a feeding tube placed into her belly next week. She came to the ER that night from the Rehabilitation facility because the IV line had stopped working. In discussions with the family, they were very concerned about the IV, yet in contrast, I was very concerned that no one knew that Mrs. Wiggins was dying…except perhaps Mrs. Wiggins herself.
I asked the family if I could have a word with them outside of Mrs. Wiggins’ room. “I wanted to talk to you about the big picture of what is going on with your mother, Mrs. Wiggins. Everything you have told me and everything that I see means that your mother is near the end of her life. These are the changes that we often see weeks and months before someone dies.”
Eyes became misty. The eldest son said, “That’s what I was afraid of.”
I continued, “We usually know this deep inside but we need to hear it from a healthcare professional to accept it.”
As I continued to talk about the path before them, the son crossed his arms, then squared his shoulders, and a firm resolve began to develop in his countenance. He opened his mouth to speak, and expectantly, I knew what he was about to say….and it was NOT this:
“Well then, let’s take her home”
Shocked and confused, I said, “Excuse me?”
He repeated himself, “Well, if she is dying, then we had better take her home to her own house.”
Without hesitation, he said, “She has been a good Mama and she always told me that she wanted to die at home, so this is the right thing for us to do for her. She took care of us, now we are going to take care of her.”
Of course I was reeling because I fully expected him to say, “Let’s get this IV fixed and get back to rehab.” But instead, this family already had some pre-set goals for the end of their mother’s journey, they just needed someone to tell them honestly “where she was” so that they could make a “U turn” off of their present path and head home to their desired destination.
Patient 2- Mr. Burrows was a humorous giant of a man, smiling despite concerning circumstances. Mr. Burrows had metastatic cancer for which he had stopped cure-focused treatment and had signed up for home hospice services. The problem was that he lived alone and was rapidly becoming unable to care for himself. That morning the hospice nurse arrived to find him on the floor where he had been lying since the day before. Unable to lift him alone and concerned about his living/social situation, she called 911 and Mr. Burrows was brought into the Emergency Department.
“How are you today Mr. Burrows?” I asked.
He smiled, “Pretty good for a man on his last leg.” He continued to make humorous quips and remarked that we had “excellent customer service here,” but he was also unable to tell me where he was or what had happened in the last week or so. It was clear that he was no longer able to take care of himself and didn’t appear to be capable of making rational decisions about his care or his future; so, I called his daughter who was listed as his power of attorney.
She was nice enough, but had no real clue how close her father was to dying. Despite being under hospice care, no one had given this daughter a clear map of the road ahead and it had not sunk in that hospice care meant that we expected him to have 6 months or less of life remaining.
So, I told her.
“You know, for your father to even be a hospice patient, this means that he isn’t expected to live more than 6 months, but I have to honestly tell you that it may be much shorter than this. He has really come to a place where all bets are off, he is far enough down this path that he may live 2 months or he may not even wake up tomorrow.”
The daughter held her hand over her mouth in shock, and a small sob escaped her lips.
Very gently, I continued: “The question we must answer today is- where can he safely and happily live out his last days? “
She responded, “I can’t let him go to a nursing home…I am going to move in with him. That’s the right thing to do…”
In this case, the mapping of Mr. Burrow’s timeline allowed his daughter to make a clear decision regarding his future care and well-being.
Patient 3- Mrs. Smith was a 67 year old female who had suffered a spontaneous brain hemorrhage about 4 months prior, which had left her paralyzed and unable to speak. Today, she was brought in from home by her family who had been caring for her there. They had noticed increasing weakness and cough (probably due to aspiration). Further, they stated that she had lost 20 lbs in 4 weeks and had started spitting out her food.
I sat her family down and this is what I said: “I want to have a “big picture” conversation with you in as gentle a way as possible. I want to talk to you like you are my family, and I need to tell you that Mrs. Smith is near the end of her life.” I paused and everyone held hands.
Her husband said, “I thought this was the case” through welling tears.
Continuing, I said, “A “bleeding stroke” with paralysis is a huge “hit” and now what we are seeing are signs of decline. She is losing weight because her appetite is leaving, and this cough is probably a sign of aspiration and is likely going to occur over and over again before she dies.” I paused to let the landmarks sink in, to become recognizable in their minds.
After I identified the landmarks, I then laid out the optional pathways for them “Now, I can attempt to treat each thing that I see, but it does not change where she is in the big picture, which is that she has entered her end of life path. Actually, if we pursue a cure-focused pathway, meaning treating each thing that arises, we may have short term success in treating the problems, but this pathway will increase the likelihood that she will die in this hospital. In contrast, if we choose comfort-focused care, meaning choosing primarily those medicines which create comfort, this will almost assure that she dies at home. The question is: What would she have chosen for herself? If we could go back in time to before the stroke, and if she could look forward into this moment and hear this conversation, what would she want for herself? What would she want us to do next?”
There was a pause, but then with clarity, her husband stated, “She would want us to just keep her comfortable and go home.”
He then shared his wife’s map with me, “You see, Doctor, we are really fortunate because she already told us what to do or not do when we got to this point, we just needed someone to tell us that we were here. We needed someone to tell us that we had arrived at the place where we could activate her wishes so to speak (to follow the pathway that she had already mapped out for them).”
These 3 patients and their families taught me to never, ever underestimate the power of a map. Knowing where you are and what to expect on the path of life sometimes changes everything.
(As always, names and elements of these patient stories have been changed to protect the privacy of the patient and the family. Date of publication has no relevance to the date of the actual patient encounter.)
Dr. Monica Williams-Murphy is a Board Certified Emergency Medicine Physician, who practices in one of the largest emergency departments in the United States at Huntsville Hospital. Through her writing and speaking, she is devoted to transforming the end of life into a time of peace, closure and healing.